History of Dental Bonding and Adhesive Dentistry
 Today, adhesive dentistry is a part of nearly every dental practice in the United States, and certainly in Illinois. The term “bonding” is used by dentists to patients with several different meanings, however the bond that is being referred to can only occur as a result of complex chemical interactions between tooth structure and the particular dental adhesive material used. When using composite resin filling materials, for example, a cosmetic or restorative dentist is basically creating a sandwich using the tooth and filling material as the bread and the bonding agent acts as the “glue” to keep the sandwich together. This portion of Glamour Smiles serves to explain the various types of bonding agents (dental adhesives) and their pros and cons.
Today, adhesive dentistry is a part of nearly every dental practice in the United States, and certainly in Illinois. The term “bonding” is used by dentists to patients with several different meanings, however the bond that is being referred to can only occur as a result of complex chemical interactions between tooth structure and the particular dental adhesive material used. When using composite resin filling materials, for example, a cosmetic or restorative dentist is basically creating a sandwich using the tooth and filling material as the bread and the bonding agent acts as the “glue” to keep the sandwich together. This portion of Glamour Smiles serves to explain the various types of bonding agents (dental adhesives) and their pros and cons.
Historically, adhesive dentistry dates back to 1955 when Buonocore thought that acids could be used as a surface treatment before adding resin to enamel.1 His work continued for over a decade, and in the 1960’s the idea of “resin tags” that connect tooth enamel to restorative resin thereby creating a micromechanical bond2 was the culmination of his work—and this idea is accepted today as the premise for modern day adhesive dentistry. Today, some dentists utilize a 37% phosphoric acid etch for a period of 15-20 seconds (some adhesives do not require this etching format, which is discussed below) when bonding. The issue which remains is that while much strength and longevity can be found when interacting resins with acid-etched enamel, it is much more of a challenge to establish this feat with dentin.
Dentin bonding is very difficult because dentin is 17% collagen by volume, but this cannot be utilized for bonding due to the hydroxyapatite crystals surrounding the collagen.3 As this is the case, all bonding to dentin must occur through the use of dentinal tubules. Each tooth has varied amounts of healthy tubules depending on a tooth’s age, restorative history, direction of the tubules, depth within the tooth, and the smear layer.4, 5 The technology that is used today is much more advanced than the initial techniques employed by Buonocore, however his discovery is the basis for modern adhesive dentistry.
Today, cosmetic dentistry is performed with the routine use of these bonding systems—however very few dentists take the time to learn and understand their impact on the longevity of their restorations. It is difficult to admit, but a fact that newer bonding systems are not necessarily better. In the opinion of general dentist Brent Engelberg, overall in the last 30 years, tooth bonding systems have basically been simplified for user convenience, and not actual bond quality. While “easier” for a dentist to place, nearly all of the newer systems have inferior bond strengths than their predecessors. Most of these new systems are marketed to dentists by dental sales representatives, without any long term clinical results to support their use.
Dr. Engelberg believes that patients deserve to receive dentistry backed by clinical research as well as long term studies and proven clinical success. The historical changes in bonding systems can be characterized by generation, and this is the format that will be used from this point forward. Today, however, many dentists characterize bonding systems as “total-etch” or “self-etch” which will be described below within each generation section.
First Generation Dental Adhesives
The first generation bonding systems were published by Buonocore in 1956 and Bowen in 1965.6, 7The idea was to take resin which contained acid and to bond this to acid-etched dentin in Buonocore’s case, however this failed when it interacted with water quickly, and the human mouth is constantly “in water” with saliva and any food and beverages that are consumed. Bowen used a bi-functional molecule (a coupling agent) where one end would bond to dentin, and other would polymerize with composite resin. Overall, this generation lead to very poor clinical results as well as low bond strengths in the 1-3 megapascal range.
Second Generation Dental Adhesives
The second generation bonding systems were introduced in the late 1970’s, and sought to improve the coupling agents that were utilized in the first generation of adhesives. The 2nd generation adhesives boasted an ionic bond to calcium in the tooth with the chemical components of the adhesive. This ionic bond would rapidly degrade in water submersion (again analogous to saliva) and even the water within the dentin itself, and cause debonding and/or micoleakage.8 The smear layer was still not removed, and this contributed to the relatively weak and unreliable bond strengths of this second generation. The smear layer is really a smooth layer is organic debris that remains on the prepared dentin surface as a result of tooth preparation with rotary instruments (the drill).
Third Generation Dental Adhesives
The third generation bonding systems introduced a very important change: the acid etching of the dentin in an effort to modify or partially remove the smear layer.9 This opened the dentin tubules and allowed a primer to be placed after the acid was completely rinsed away. While this method achieved a greater bond, it was considered controversial in dentistry as the feeling existed that dentin ought not be etched. After the primer was added, an unfilled resin was placed on both dentin and enamel. The weak link with this generation was the unfilled resins—they simply did not penetrate the smear layer effectively.
Fourth Generation Dental Adhesives
The fourth generation bonding systems were introduced in the 1990’s, and many dentists still utilize them today—including Chicago suburban cosmetic dentist Dr. Brent A. Engelberg. Fourth generation was the first to achieve complete removal of the smear layer. Third generation adhesive techniques altered this layer, but did not remove it. The total-etch technique is a major aspect of the 4th generation systems, where dentin and enamel are etched at the same time with phosphoric acid (H3PO4) for a period of 15-20 seconds.10 After this step, the acid is rinsed, leaving exposed and demineralized dentin that can be filled with primers and resins. The depth and degree of infiltration of the “collagen network” within the dentin is the most important factor in the quality and predictability of the bond.14 The hybrid layer is formed by the resin-infiltrated dentin and is neither resin nor dentin, but a hybrid of the two.3 The goal of ideal hybridization is thorough penetration of the resin into the demineralized dentin and engagement of the underlying and still mineralized dentin.15
Fourth generation adhesives involve a total etch and rinse, application of a primer and adhesive that have been mixed together just prior to placing, and then light curing the tooth. Brand name examples are Optibond FL, Scotchbond, and All Bond 3. All Bond 3 (manufactured by Bisco in Schaumburg, Illinois) is a dual-cured, 3 step universal dental adhesive system that is compatible with all dental materials, is hydrophobic in nature, and is composed with an ethanol-based solvent. General dentist Brent Engelberg typically uses this adhesive because of its proven track record, and his ability to achieve an exemplary level of clinical success with thousands of bonded porcelain and composite restorations.
Excerpt slide from a lecture by Dr. Brent Engelberg on adhesion illustrating the basic chemistry differences between generations four through seven.
A complication with 4th generation adhesives is that the acid, when rinsed, must be effectively rinsed without over-drying the tooth. The desired “moist dentin” must remain for proper “wet bonding” with this method, and there are strong technique sensitivity requirements for this to work.11, 12 Only an experienced cosmetic dentist can predictably achieve proper bonds and zero post-operative sensitivity with this technique. The reason for this issue is that the inorganic portion of the dentin (hydroxyapatite matrix) is dissolved when etching, in essence removing the scaffolding which supported the collagen fibrils. These very fibrils are needed to construct an effective hybrid layer, and must be rehydrated or not over-dried when the phosphoric acid is rinsed away. However, in the right dentist’s hands, no adhesive system invented since the 4th generation has achieved equally successful hybrid layers, resin tags, lateral branches, overall seal, and therefore higher longterm bond strengths.13
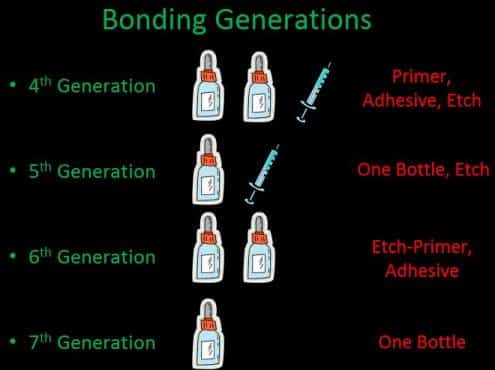
Excerpt slide from a lecture by Dr. Brent Engelberg on adhesion illustrating the basic chemistry differences between generations four through seven.
Fifth Generation Dental Adhesives
The fifth generation bonding systems sought to simplify the process of fourth generation adhesion, and combined the primer and adhesive into one bottle. In effect shortening the working time when performing a procedure as well as potentially eliminating error in this now removed mixing step. In addition, the question “how wet it wet” was essentially eliminated. Moist bonding should still be used, and the collagen still collapses when the dentin is dried after etching and rinsing. Nearly all dental dual-cure crown build up materials are not compatible with this generation of adhesive (with the exception of Bisco’s ‘One Step’ 5th generation adhesive). It is important that a dentist understand this chemistry along with the paired restorative materials that they are using in order to ensure clinical success. Several long term studies indicate that 5th generation dental adhesives achieve high clinical bond strengths. Dr. Engelberg has used and had success with this generation of adhesive for many years—and the simplification of eliminating one step in the application process was appreciated as the clinical results were proven to be outstanding.
Fifth Generation adhesives involve a total etch and rinse, application of a primer and adhesive that are already mixed, and then light curing the tooth. Brand name examples are Excite, One Step, and Adper Single Bond.
However when compared in a 4-year water study (the mouth contains water at all times in the form of saliva) side-by-side with fourth generation adhesive, the 5th generation adhesive had a significant decrease in bond strength.16 The results summarize that in a clinical situation, a 4th or 5th generation adhesive can achieve reliable dentin bonding if all preparation margins are on enamel, however if any of the margin involves dentin, a 4th generation adhesive is preferred. The norm is that dentin is involved, therefore Dr. Engelberg prefers 4th generation adhesives exclusively today—even though the technology was developed for the initial versions of this generation nearly 30 years ago! In addition the resin-dentin bond is prone to water degradation, 5th generation adhesives are more prone to water degradation than 4th generation dental adhesives.16
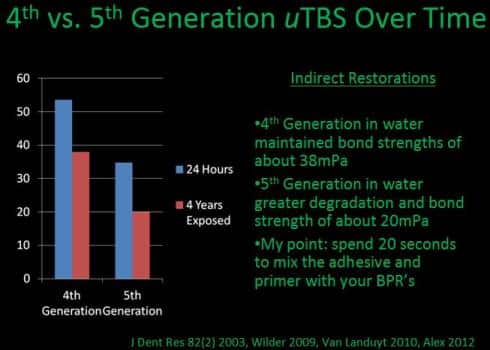
Excerpt slide from Dr. Brent Engelberg’s lecture on adhesion demonstrating the benefits of 4th Generation Adhesives over 5th Generation Adhesives over time. Note the 5th Generation strength drop-off after four years.
Sixth Generation Dental Adhesives
The sixth generation bonding systems sought to eliminate the etching step, or to include it chemically in one of the other steps. The sixth-generation adhesives require no etching, at least on the dentin preparation surfaces. The quality of the bond after aging in the mouth remains strong to dentin after time, while it is the bond to the unetched and unprepared enamel is suspect. Additionally, the multiple components and multiple steps in the various sixth-generation techniques can cause confusion and lead to error. There have also been some concerns about the efficacy and predictability of various innovative mixing procedures. Bisco’s ACE systems ease mixing concerns, for example ACE All Bond SE is a 6th generation, type II bonding agent that actually combines unmixed portions of the chemistry when the dentist “clicks” on the cartridge dispensing system in a perfect ratio. In addition, when mixed in the well in which the liquids are deposited, a pink color appears which notifies the clinician that the chemistry is active and proper for use.
Sixth Generation adhesives involve the application of an etch-primer which has already been mixed followed by an adhesive application prior to light curing the tooth. Brand name examples are Clearfil SE, Prompt L Pop, and ACE All Bond SE.
While data indicates that 6th generation adhesives will adhere well to dentin (41 MPa at 24 hours), the bond to enamel is at least 25% weaker to enamel then both the 4th and 5th generation adhesives in pooled data studies.17 Several respected clinicians have utilized 6th generation adhesives for bonding to dentin after selectively etching the enamel, or combining this 6th generation chemistry with Pascal Magne’s “Immediate Dentin Sealing Technique,” however this only works in cases with specific provisionalization techniques are not utilized, and really tap dances around the proven 4th generation adhesive results to both dentin and enamel with no additional techniques.
Seventh Generation Dental Adhesives
The seventh generation bonding systems sought to eliminate all steps prior to adhering composite or porcelain restorations. Every step is completed using only one bottle of liquid which contains the etch, primer, and adhesive. It was very exciting when these products first came to market as the claim was that you could achieve consistent bond strengths while completely eliminating the errors that could normally be introduced by the dentist or dental assistant who had to mix the separate components with other more complicated systems. The good news was that this was completely true—there was not any mixing required and the bond strengths were consistent. The bad news is that 7th generation adhesives have proven to have the lowest initial and long term bond strengths of any adhesive on the market today. Surprisingly, these adhesives are among the more commonly used in practice in the United States today. In fact, as recently as 2011, 4th and 5th generations adhesives combined were sold equally as much as 6th and 7th generation adhesives combined in the U.S.A.15
Seventh Generation adhesives involve the application of the etch, primer, and adhesive which have already been mixed, followed by light curing the tooth. Brand name examples are iBond, G Bond, and Bond Force.
Seventh generation adhesives are “all-in-one” if there has ever been such a thing. The clinical and scientific data on these adhesives proves that they are hydrophilic and degrade more rapidly. In addition, because of the inclusion of so many components into one bottle, these systems need to have a higher amount of solvent (the carrier for the chemical components of the system, usually alcohol or water today), which limits the depth of resin infiltration into the tooth and can create voids.17 In addition, the chemistry must be acidic, as etch is involved in this liquid, and this has been shown to adversely react with the composite initiator systems.17
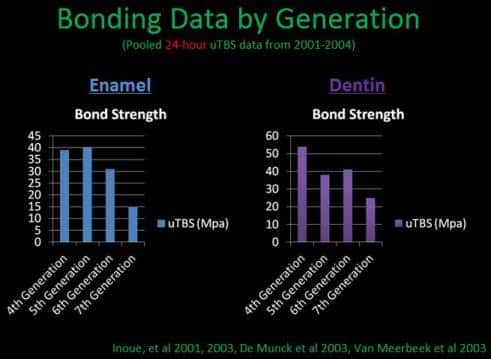
Excerpt slide from Dr. Brent Engelberg’s lecture on adhesion demonstrating Enamel and Dentin Bond Strength by Generation.
Universal Dental Adhesives
Newer to the marketplace, the so called “universal adhesives” have been used since 2011 in clinical practice. The first two major brand names for this category of adhesive are Bisco’s All Bond Universal and 3M’s Scotchbond Universal. This class of adhesives utilizes MDP, which is hydrophobic in comparison to the previously hydrophilic 7th generation adhesives. As the main culprit in adhesive breakdown is water (hydrolysis), it makes more sense to utilize an adhesive that is more hydrophobic: literally “water fearing,” but this clinically means that it repels water. 3M’s version of the product requires a separate activator for dual and self-curing materials, which is an extra step. In addition, selective etching of the enamel is recommended for a better bond to enamel. Dr. Engelberg questions the point of an adhesive that can require just as many steps as a 5th or even 4th generation adhesive when you could just use a 4th or 5th generation adhesive that is more clinically studied long term. While the advancement of 7th generation adhesives with the addition of MDP is promising, there is no data to support the use of these products on Dr. Engelberg’s cosmetic dentistry patients at this time.
Matrix Metalloproteinases (MMP’s)
Matrix Metalloproteinases are enzymes that degrade the organic matrix within dentin after acids have been applied. Etching will dissolve the inorganic matrix and cause the collagen to collapse—which can be rehydrated with wetting in order to have an effective hybrid layer with the organic layer’s collagen. Even if this is the case, if MMP’s are able to eat away the collagen layer alone, then adequate hybrid layer formation is not possible, and hydrolysis would cause a more rapid breakdown of the hybrid layer. New studies have shown that antimicrobial solutions containing chlorhexadine and/or benzalkonium chloride actually will inhibit MMP’s.38, 39, 40 As this is the case, Dr. Engelberg always applies a chlorhexadine-based pumice to all teeth before bonding. The use of pumice combined with chlorhexadine (Consepsis from Ultradent) on teeth before porcelain veneers, crowns, or even composite resins are placed using an adhesive protocol is an extra step that is proven to increase the bond strength for many reasons, including: removal of plaque and bacteria, inhibition of MMP’s, removal of provisional cement, removal of preparation debris, and a decrease in secondary decay potential. All Northwest and North Suburban Chicago dental patients of Dr. Engelberg are aware of his devotion of this additional step that improves clinical results for his cosmetic and general dental patients.
Which Dental Adhesive System is the Best?
According to Gary Alex, the “ideal” adhesive system would be one that is hydrophilic when first placed to interact with dentin, which has inherently high water content, but then become completely hydrophobic once polymerized to discourage water sorption and hydrolysis. Unfortunately, no such chemistry currently exists. Therefore, the next best choice would be a graduation from hydrophilic to hydrophobic while moving from the tooth tissues to the interface with the restorative material. This is basically the strategy used by the 4th and many 6th generation adhesive systems, which involve the placement of hydrophilic primers that are then overlaid with more hydrophobic resins.15 This rationale coupled with the ability of 4th generation systems (total etch and rinse) to bond with enamel more effectively then 6th generations systems17, Dr. Engelberg absolutely selects a 4th generation system (All Bond 3) as his bonding agent of choice. There are technique sensitivity and time concerns with 4th generation systems, however the compromises that are made in clinical results should not offset the use of 4th generation systems even with today’s vast dental adhesive choices.